Once the patient has been evaluated and deemed a good candidate for the Reference Denture Technique, the clinician must then evaluate the patient’s current dentures. Are the extensions of the denture base appropriate for the anatomy of the patient? Have the teeth worn and had the occlusal vertical dimension closed because of it? Are the bases coving the tuberosity of the maxilla and the retromolar pages of the mandible? Are all the basic criteria that make a successful denture found in the patient's current prosthesis? The clinician must make the decision that the current denture can be used as the foundation for the new prostheses.
In the denture illustrated here, all the criteria have been met. The patient reports that the dentures have served them well for the last 10 years. The extensions of the maxillary and mandibular bases appear to be appropriate for the patient. The teeth, although worn are in the appropriate exposition, the occlusal plane bisects the dentures and appears to be in alignment with the patient's anatomy. In this case, both the patient and the clinician were happy with the position and esthetics of the dentures and no radical changes are required. The vertical horizontal and vertical overlap appear to be appropriate. This is an ideal denture for the reference denture technique.



The length, width, and position of the final borders should represent the final shape of the denture. This is not always easy to accomplish but it should be your goal. This makes it much easier for the technician to create a digitally fabricated occlusal base, BTI, or WTI.
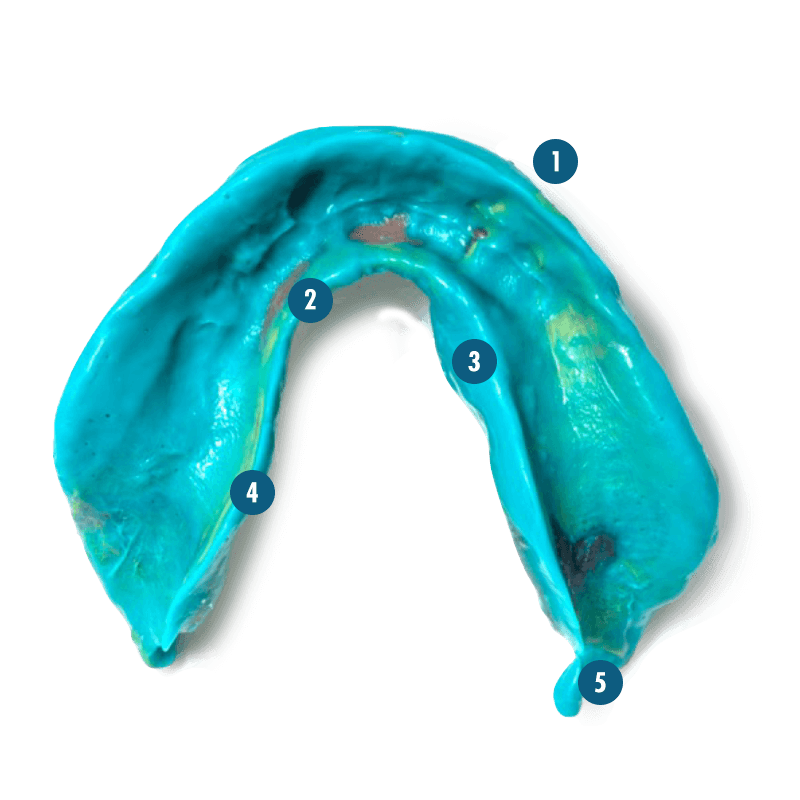
You will still have “show throughs” in the final impression.
The technician can quickly correct over-extensions of the flanges and cameo surface if they have examples of well-formed borders in other parts of the impression.
In this example, the S-shaped curve is fully developed
Extra material can easily be trimmed away prior to scanning the impression.
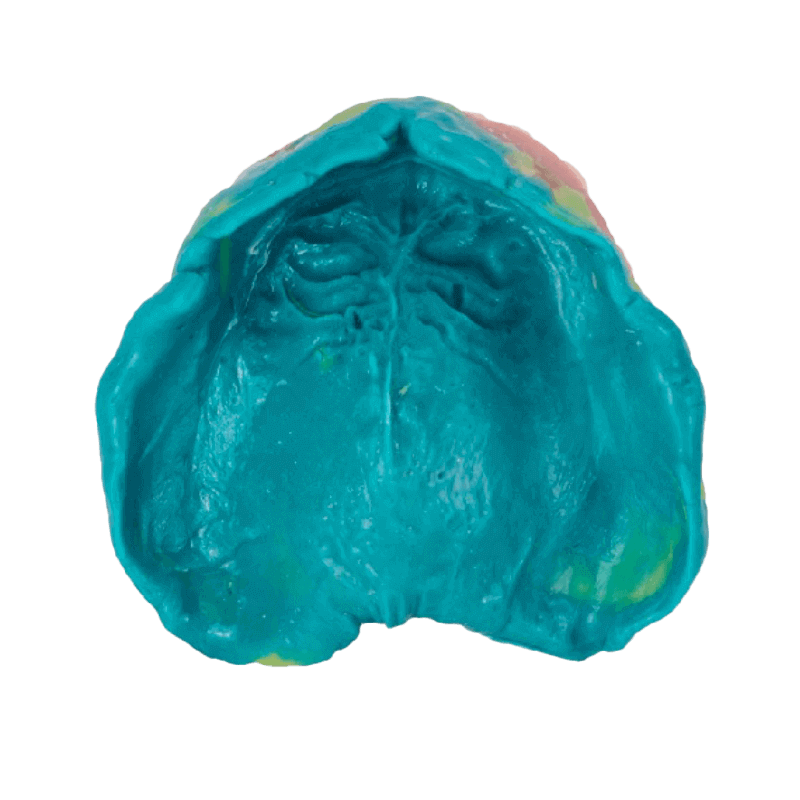
Repeat the process for the maxillary impression.

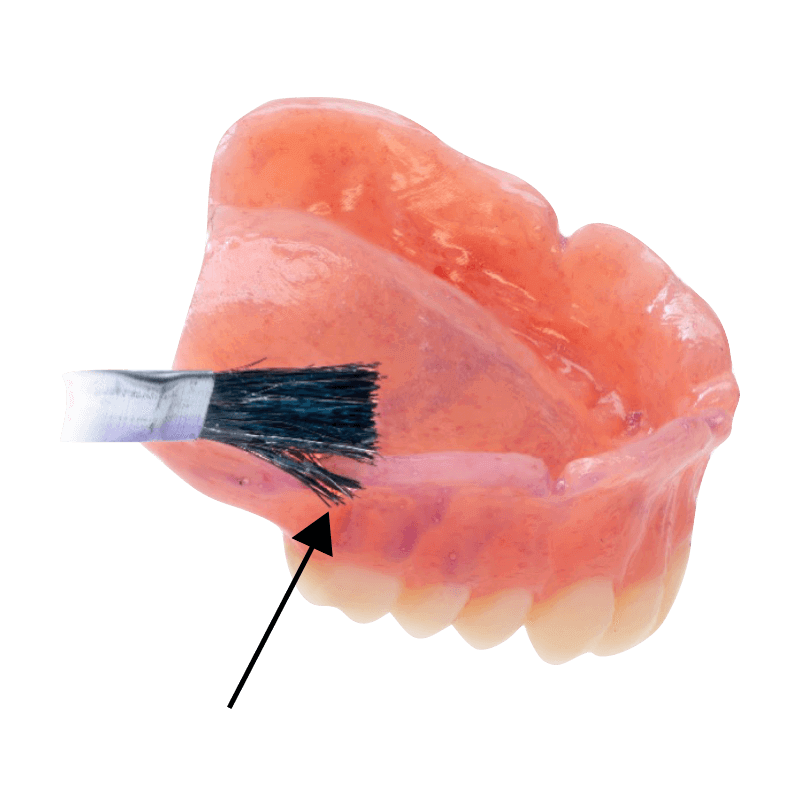
Once the impression is finished, any impression material would interfere with making an interocclusal record. Remove excess material with a Bard Parker Blade.
In some instances, additions to the posterior portion of the denture will interfere with closure against the maxillary denture and impression. These areas must be carefully evaluated.
Scan the maxillary and mandibular dentures using an intraoral scanner.

Several photographs are routinely taken for use by the technician. Illustrated here is a close up of the patient in occlusion. The lips are parted and this allows the technician to have some sense of the tooth positions relative from the maxilla and mandible. The exposure of the maxilla and mandibular teeth, the buccal corridor, occlusion, and lip support

Retractors are used to display the entire denture of the oral cavity. This allows the technician to get a sense of the occlusal planes, have a sense of the extensions of the denture, the negative space created around the denture, and the appropriateness of the plane of occlusion.
the Fox plane held with a resin seal at place in the patient's mouth can be photographed in both the anterior and lateral positions. This allows the technician to get a sense of the horizontal plane comparing the Fox plane to the pupils of the patient. The lateral shock can give a sense of the anterior posterior plane that would be represented by the connection of a line parallel to Camper's plane, which goes between the ala of the nose and the tragus of the ear. These photographs can be used by the technician to modify the occlusal point if necessary, or at least confirm the plane as it is currently set.

The occlusion can be checked, evaluated, and modified on the monolithic denture. Any changes made here will be duplicated in the final prosthesis.
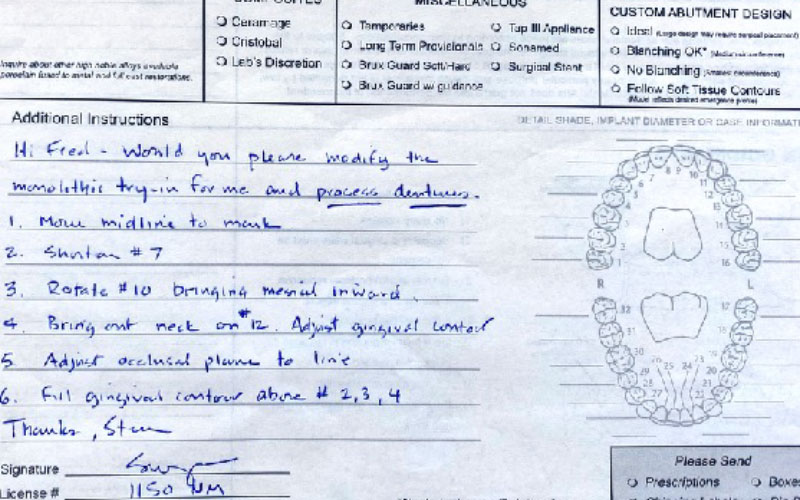
Notes are taken on the prescription form and they typically reference the photos and photos of the monolithic denture as they will be marked using a Sharpie pen.

One of the disadvantages of the monolithic dentures, the inability to move teeth and wax. This can be a reason not to use a monolithic denture in certain circumstances. Specifically when the patient is very aware of the aesthetics and the prosthesis is very demanding and would best be served by seeing a trial denture that has both independent teeth and gingival colored wax.
The best way to communicate with the trial denture to the technician is to, one, re scan the denture, following any modifications made to the occlusion or to the tissue surface itself, or by using photographs taking of the monolithic denture marked with a Sharpie. And this illustration, we could see that it was suggested that the midline be moved to the left, tooth number two rotated, tooth number 13 possibly have the buccal portion of the tooth placed buccally. Over teeth number three, it was suggested that more wax contour be positioned there.

the circle over teeth numbers three and four indicate the need for a filling of the contour in that area.
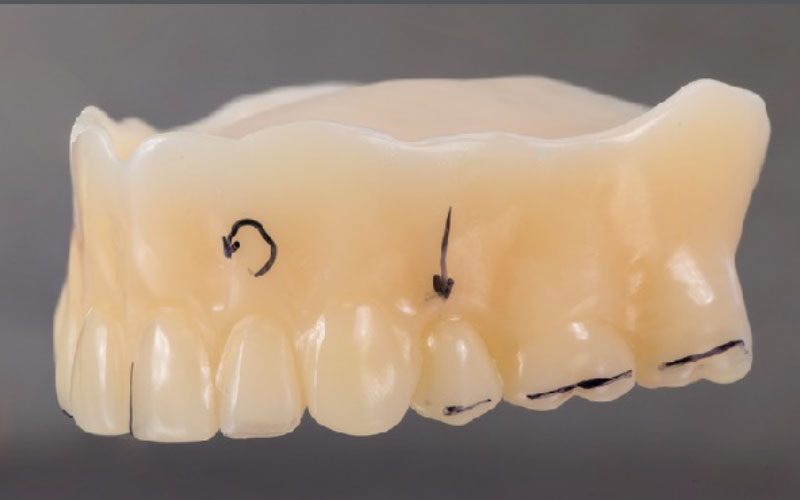
The Sharpie indicates the change of the anterior, posterior plane of occlusion, the need to reposition tooth number 12 and the request to rotate tooth number 10.

One of the important advantages of a monolithic try-on is the ability for the patient to wear the prosthesis home short term and evaluate the fit, aesthetics, and function of the prosthesis prior to constructing the final prosthesis, to be delivered at appointment three.
In this illustration, the technician has added gingiva-colored resin to the prosthesis, creating a better sense of the final prosthesis as the patient work over several weeks. In some cases, this may not be a good idea.
It's been said that there have been patients that have decided that this prosthesis was good enough for them, and they didn't return for the final prosthesis. This is unfortunate for several reasons. The material is not designed for long-term use, and you can have significant wear of the occlusion over months.

This is an example of a trial denture that was worn by the patient for several weeks. He returned to the office with a comment that he liked the aesthetics of the prosthesis, he felt that the maxilla prosthesis was very retentive and he was pleased, but he did feel that the mandibular denture was not as retentive as possible. At this point, a new final impression was made using Aquasil Ultra + LV and that was in turn, judged by the patient to be more retentive.

Following the approval by the patient and the approval by the clinician, the monolithic dentures are then scanned using an intraoral scanner. All surfaces are scanned; the intaglio surface, the cameo surface, and the occlusal surface of each. The interocclusal record is made using a buccal bite intraorally and that data is then sent to the laboratory. If the prosthesis were satisfactory and no adjustments were needed, the secondary scan is not necessary; rather, it is reported to the technician to base the final prosthesis on the existing model of the denture and the final denture is then constructed.

The dental technician then modifies the prothesis based on the data collected appointment two.

The final prosthesis is constructed using either milling or printing techniques. This should be an exact replica of the model of the dentures, and the changes made to that denture appointment two.

The great advantage of modifying the monolithic denture appointment two is that the final prosthesis rarely needs to be touched. Occlusion might need to be finessed, but the prosthesis itself should fit just like the final prosthesis, as the monolithic prosthesis. This is a great advantage of the digital workflow.